Resident Research
We provide mentored training in research and scholarship to individuals during several phases of their educational and professional training to develop independent and sustainable academic careers in basic, clinical, and/or translational research. Trainees include undergraduate and graduate students, medical students, post-doctoral fellows, and surgical residents and fellows in Otolaryngology/Head and Neck Surgery.
Research Training
Research training is supported by several NIH training grants. In particular, the R25 Research Education Grant (which followed our long-standing T32 training grant) from the National Institute of Deafness and Communication Disorders at the NIH supports each resident to conduct mentored research for one year during.
Resident trainees select and conduct research projects based on their interests. Projects can reside within established areas of research in the Department, described above, or they can address new avenues of inquiry via collaborations with mentors outside of the Department.
It is our goal is to provide trainees with the skills they need to develop an independent and sustainable research program in areas relevant to Otolaryngology/Head and Neck Surgery with the ability to:
- Design and execute hypothesis-driven research
- Effectively present findings to the public, in oral and written forms
- Write applications for research funding
Many clinical research trainees earn a certificate or masters degree in clinical research methods and collaborative approaches to address a wide variety of research problems.
Training Sites and Facilities
The Virginia Merrill Bloedel Hearing Research Center and the Health Sciences Building at UW have several laboratories conducting basic science and translational research. Within these sites, there are state-of-the-art imaging centers, surgical suites, tissue culture facilities, histology and microtomy suites, equipment for genetic and molecular analyses, electrophysiological measurements in vivo and in vitro, large-scale drug screening, and detailed auditory and vestibular functional testing.
The Otolaryngology Outcomes Research Group performs clinical research and is based in the UW Comparative Effectiveness, Cost & Outcomes Research Center, an interdisciplinary, multi-school clinical research “laboratory.” These Centers are closely affiliated with the UW School of Public Health and UW Institute of Translational Health.
The Fred Hutchinson Cancer Research Center houses laboratories for basic science and translational research, focusing on head and neck cancer, epithelial tumor biology, and viral biology as it relates to carcinogenesis, immunotherapy, and population studies.
There are innumerable other research facilities where departmental and trainee research is performed. For example, Seattle Children’s Hospital houses research programs on vascular anomalies, pediatric communications disorders, and others. The Department of Electrical Engineering at UW houses an engineering research laboratory studying robotic surgical techniques. The Research & Development (R&D) Program at the VA Puget Sound Health Care Center houses numerous research programs and project, and Harborview Medical Center houses the Harborview Injury Prevention & Research Center and many other research programs.
Visit the Research Resources page for links to these sites and for other helpful information.
Resident Research Highlights
Molecular Subclassification of Mammalian Vestibular Ganglion Neurons Using Single-Cell Transcriptomics
Rahilla Tarfa, MD, PhD
 Vestibular ganglion neurons (VGNs) play a critical role in the transduction of head motion to the brain, yet their molecular diversity and potential functional subtypes remain poorly characterized. Understanding this heterogeneity is essential for linking specific neuron types to vestibular functions and for elucidating how genetic and environmental perturbations may disrupt vestibular signaling. Traditional approaches, such as immunolabeling and electrophysiology, have offered limited resolution in classifying VGNs. Single-cell RNA sequencing (scRNA-seq) has emerged as a transformative tool for uncovering transcriptomic diversity at cellular resolution, yet its application to vestibular ganglion biology remains lacking.
Vestibular ganglion neurons (VGNs) play a critical role in the transduction of head motion to the brain, yet their molecular diversity and potential functional subtypes remain poorly characterized. Understanding this heterogeneity is essential for linking specific neuron types to vestibular functions and for elucidating how genetic and environmental perturbations may disrupt vestibular signaling. Traditional approaches, such as immunolabeling and electrophysiology, have offered limited resolution in classifying VGNs. Single-cell RNA sequencing (scRNA-seq) has emerged as a transformative tool for uncovering transcriptomic diversity at cellular resolution, yet its application to vestibular ganglion biology remains lacking.
With the support of a multidisciplinary team of mentors, Dr. Tarfa’s research focuses on the transcriptomic and anatomical classification of VGNs using scRNA-seq. Her mentors include Jennifer Stone and David Raible, and collaborator LiTao Tao, PhD at Creighton University. Leveraging her NIH F32 fellowship and American Otological Society funding, Dr. Tarfa has integrated datasets from adult mice to identify molecularly distinct VGN subtypes. Through rigorous data curation, and various bioinformatic analytical tools, she has characterized clusters of neurons and glial cells that reflect potential functional subgroups, with the ultimate goal of analyzing how they correlate to hair cell inputs, synaptic morphology and ganglion neuron somatic properties.
Dr. Tarfa is further exploring ligand-receptor interactions between VGNs and utricular hair cells to identify candidate signaling pathways involved in neuron-hair cell communication and synaptic refinement. She also incorporates complementary in situ hybridization and immunocytochemistry approaches to validate transcriptomic findings. By merging computational and experimental techniques, her work aims to define a molecular taxonomy of VGNs that can serve as a foundation for future studies of vestibular development, function, and disease.
This work builds on a rich legacy of sensory neuroscience at the University of Washington and exemplifies the power of multidisciplinary collaboration. Dr. Tarfa is excited to continue developing this VGN atlas as a resource for the field, with the ultimate goal of enabling targeted repair or regeneration strategies for vestibular disorders.
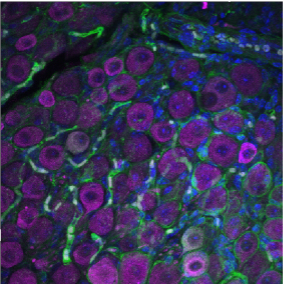
Slice of vestibular ganglion tissue, with neurons labelled with Mbp antibody, nuclei with DAPI and Map2 antibody.
Characterization and Diagnosis of Tracheomalacia Utilizing Computational Fluid Dynamic Techniques
Hannah Case, MD
 Tracheomalacia is a common congenital trachea malformation characterized by an increased compliance of the trachea, making it more susceptible to dynamic and static collapse. Thorough history and physical examination are a paramount component in the diagnosis of tracheomalacia with bronchoscopy serving as the current diagnostic gold standard. However, this diagnostic standard is subjective, user dependent, and limited in its quantification of dimensional abnormalities. Alternatively, Dynamic Airway 4D CT combined with computational fluid dynamic testing demonstrates potential for quantification of how airway shape and size restricts airflow.
Tracheomalacia is a common congenital trachea malformation characterized by an increased compliance of the trachea, making it more susceptible to dynamic and static collapse. Thorough history and physical examination are a paramount component in the diagnosis of tracheomalacia with bronchoscopy serving as the current diagnostic gold standard. However, this diagnostic standard is subjective, user dependent, and limited in its quantification of dimensional abnormalities. Alternatively, Dynamic Airway 4D CT combined with computational fluid dynamic testing demonstrates potential for quantification of how airway shape and size restricts airflow.
With support of multidisciplinary mentors, Dr. Hannah Case’s research has focused on developing a toolbox to better quantify tracheomalacia. Her team of mentors includes Alberto Aliseda, PhD (UW Department of Mechanical Engineering), Tanya Meyer, MD (UW Otolaryngology-HNS), Randall Bly, MD (UW Otolaryngology-HNS), Seth Friedman, PhD, and Mike Barbour, PhD (Seattle Children’s Hospital Center for Respiratory Biology and Therapeutics). Working with a robust team of specialists has made it possible to model and quantify the collapse events of tracheomalacia throughout the respiratory cycle and further quantify how the changing morphology impacts flow. The Multiphase & Cardiovascular Flow Lab led by Dr. Aliseda has robust experience working with various residents in the Department of Otolaryngology in modeling fluid dynamics in upper airway disease processes. The lab worked with recent UW fellow, Clare Richardson, MD, on Analysis of Upper Airway Flow Dynamics in Robin Sequence Infants Using 4-D Computed Tomography and Computational Fluid Dynamics and is currently collaborating with current resident, Shaunak Amin, MD, on Surface Reconstruction of the Pediatric Larynx via Structure from Motion Photogrammetry: A Pilot Study.
Dr. Hannah Case is fortunate to be the lab's newest mentee and is excited to be applying these principals to more dynamic respiratory pathologies. Through this project, the lab hopes to develop quantitative diagnostic modalities and expand upon our understanding of how the unique tracheal geometries of tracheomalacia impact airflow for tracheomalacia patients.
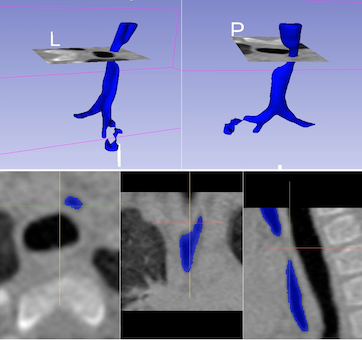
Tracheomalacia modeling