Speech-Language Pathology
Overview
Our speech-language pathologists specialize in state-of-the-art management of voice, upper airway, swallowing and facial nerve disorders. We work as part of a multidisciplinary team including laryngologists, head and neck surgeons, facial plastics and reconstructive surgeons, and other providers to provide the individualized and comprehensive care that our patients need.
Treatment options provided by our specialists
Management of voice disorders:
Our speech-language pathologists provide comprehensive evidence-based evaluation for voice disorders including auditory perceptual voice evaluations, acoustic analysis, and laryngeal videostroboscopy as well as treatment for a variety of structural, neurogenic, and functional voice disorders. We have specialists who focus on throat pain related to muscle tension and manual techniques to relieve pain, including circumlaryngeal massage and intraoral massage.
We also have a team of performing voice specialized speech pathologists who care for singers, actors, voiceover artists and other performers. They offer voice therapy specific to the performer’s needs and work in a multidisciplinary clinic to provide integrated care. Please see Performing Voice Clinic · UW Otolaryngology Head & Neck Surgery.
Management of swallowing disorders:
Our speech-language pathologists provide state-of-the-art evaluations for swallowing disorders including videofluoroscopic swallow studies, flexible endoscopic evaluation of swallowing, and high-resolution pharyngeal manometry. Highly specialized and personalized treatment plans are created for each patient to ensure maximal rehabilitation using head/body positions, swallowing strategies, diet modifications, biofeedback (including visual biofeedback through high resolution pharyngeal manometry for strengthening and sequencing, submental EMG, and bioFEESback), home exercise swallowing programs, and intensive bolus and device-driven exercise programs.
Management of head and neck cancer:
Speech-language pathology is an integral part of a comprehensive multidisciplinary model for head and neck cancer management. Our team works closely with head and neck surgeons, radiation oncologists, medical oncologists, and other supportive care professionals to provide preventative and rehabilitative services aimed at maximizing quality of life as well as long term swallowing and communicative function before, during, and after treatment. We offer specialized care for alaryngeal voice restoration after total laryngectomy, lymphedema, trismus, oral prosthetics, and radiation-associated dysphagia.
Management of upper airway disorders:
Our speech-language pathologists also specialize in the care of patients with laryngeal hypersensitivity, chronic cough, chronic throat clearing, inducible laryngeal obstruction (or paradoxical vocal fold motion), and laryngospasm. We provide specialized respiratory retraining and behavioral cough suppression therapy to significantly improve quality of life for our patients.
Gender affirming voice care:
Our goal is to help our transgender, non-binary, two-spirit, and gender non-conforming patients achieve a voice that aligns with and affirms their gender. For most patients, the first step towards gender-voice alignment is to engage in gender affirming voice therapy with our speech pathology team. During gender affirming voice therapy, you and your speech pathologist will develop individual voice goals and engage in exercises that assist you with achieving those goals. Potential areas for exploration in voice therapy include voice sustainability, resonance, pitch, and speech patterns. It’s important to note that voice therapy is for people of all genders, and anyone experiencing voice-gender incongruence is appropriate to participate in care. Gender affirming voice surgery with our laryngology team may be considered following voice therapy. For individuals who have completed voice training elsewhere, it’s important to note that pre-operative and post-operative voice therapy is still necessary to develop increased vocal control and flexibility to maximize the success of any surgical interventions.
Facial neuromuscular retraining:
When a person suffers from injury to the facial nerve, we provide specialized facial neuromuscular retraining to help improve functional outcomes for those with facial paralysis, paresis, or synkinesis. Evaluation and treatment of facial nerve disorders is collaborative and multidisciplinary, where treatment is often completed in adjunct with our facial plastic and reconstructive surgeons Facial Nerve · UW Otolaryngology Head & Neck Surgery.
Providers
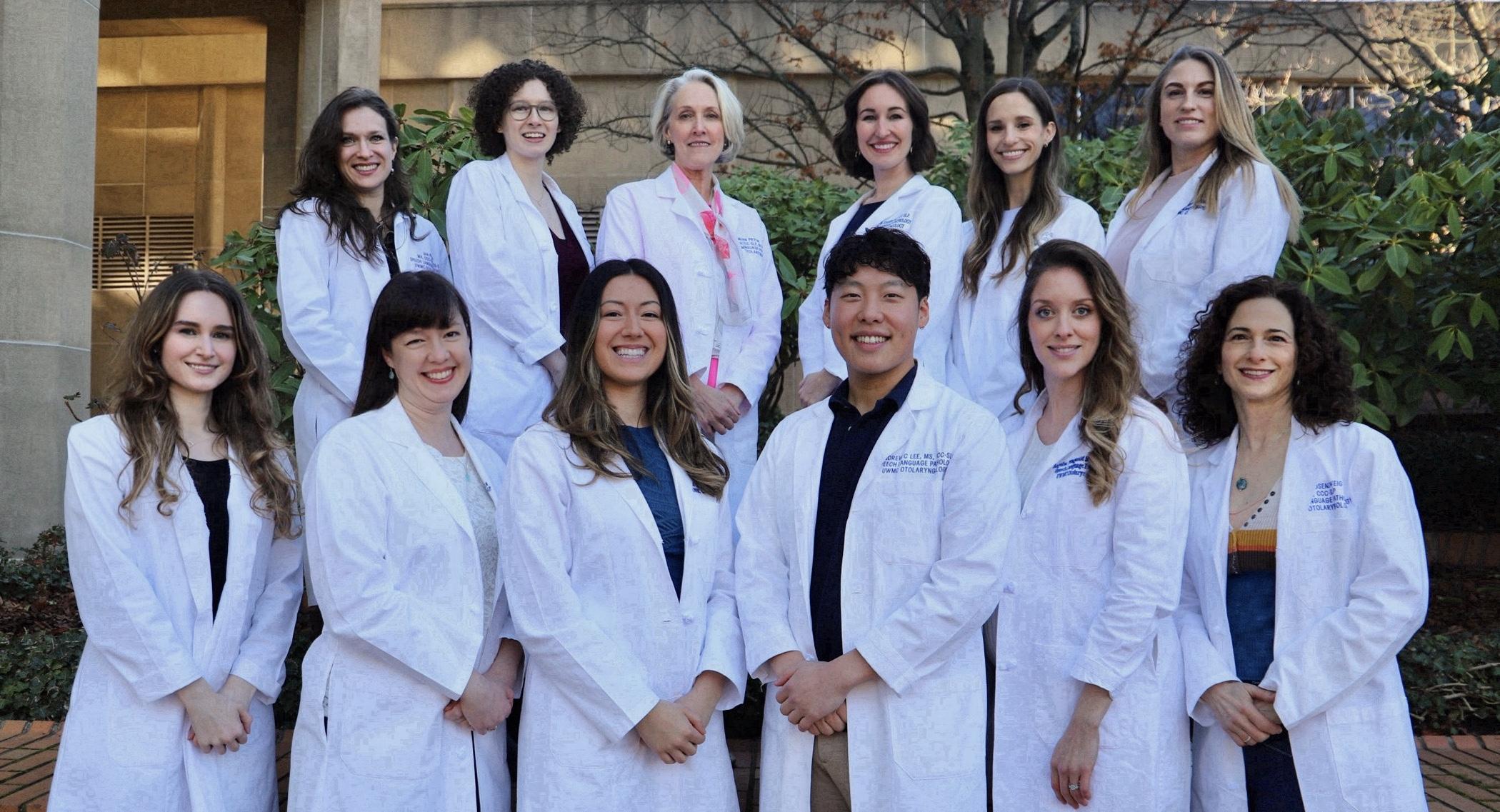
Top row, from left: Abby Eagleson, MS, CCC-SLP; Jess MacKimm, MS, CCC- SLP; Jan Pryor, PhD, CCC-SLP, BCS-S; Lisa Zughni, MS, CCC-SLP; Emily Wilson, MS, CCC-SLP; Rebecca Hayes, MS, CCC-SLP. Bottom row, from left: Madeline Knutson, MS, CF-SLP; Alison Hirst, MS, CCC-SLP; Haley Wilcox, MS, CCC- SLP; Andrew Lee, MS, CCC-SLP; Angelina Fitzgerald, MS, CCC-SLP; Juli Rosenzweig, MS, CCC-SLP.
Faculty Providers
Lisa Zughni, MS, CCC-SLP
TEACHING ASSOCIATE; DIRECTOR OF SPEECH LANGUAGE PATHOLOGY
Clinics
Otolaryngology-HNS at UW Medical Center - Montlake
Our highly trained surgeons, providers, nurses and support staff treat patients with disorders such as chronic sinusitis, dizziness, cancer and the loss of ability to hear, speak and/or swallow.